The Dual Role of the Pediatric Oncology Nurse: Compassion, Competency, and Critical Care
Published: 17 Oct 2025

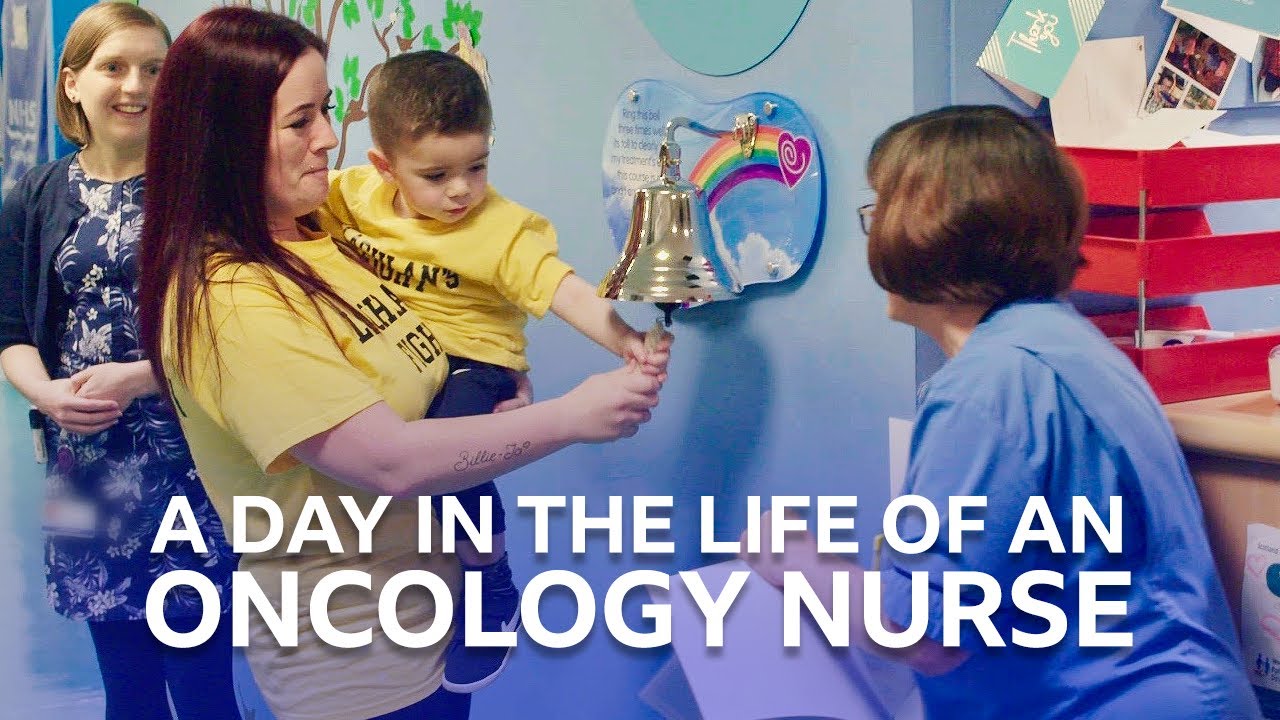
Pediatric oncology nurse is a pillar support in managing Pediatric cancer. Diagnosis of cancer in a child shatters a family’s world, placing them on a complex path filled with high-stakes medical decisions, intense treatments, and profound emotional strain. In this highly specialized environment, one professional acts as a constant anchor, possessing a rare duality of world-class clinical expertise and deep, unwavering compassion: the Pediatric Oncology Nurse (PON).
A PON (Pediatric Oncology Nurse) is far more than a caregiver; they are a highly specialized clinician, an educator, a crisis navigator, and a psychological sentinel. This blog post dives into the essential competencies that define this role, establishing why the Pediatric Oncology Nurse is central to the success of family-centered care.
What do the pediatric Nurses do?:,The Pillars of Specialized Competence.
To successfully manage the complex, rapidly evolving nature of childhood cancer treatment, the PON( Pediatric Oncology nurse)must demonstrate a set of clinical competence and technical proficiency that goes beyond general pediatric nursing. This specialization is the bedrock of their practice, positioning them as an indispensable member of the interdisciplinary team.
- Advanced Clinical and Technical Proficiency
The treatments for pediatric cancer—including chemotherapy, radiation, surgery, and especially Bone Marrow Transplants (BMTs)—are complex and carry significant risks. - Chemotherapy Administration: The PON is the primary administrator of potent cytotoxic agents. This requires advanced knowledge of specific drug protocols, rigorous safety standards (per Oncology Nursing Society guidelines), and the management of central venous access devices (CVADs).
- Precision in calculation, preparation, and infusion is non-negotiable, as even minor errors can have catastrophic consequences for a child’s tiny body.
- Symptom and Side Effect Management: Childhood cancer treatments bring a host of debilitating side effects, from severe nausea and vomiting to life-threatening neutropenic fever, mucositis, and severe pain. The PON must possess expert knowledge in targeted symptom management protocols, utilizing advanced pain control methods and quickly identifying subtle signs of patient deterioration, which is crucial for improving patient outcomes and quality of life.
- Infection and Blood Product Management: Due to compromised immune systems, children with cancer are highly vulnerable. PONs are experts in meticulous infection control and the rapid, safe administration of blood products (plKnown to meates, red blood cells), demanding specialized training in hematology and transfusion reactions.
The Pillars of Specialized Competence in pediatric oncology nursing
To successfully manage the complex, rapidly evolving nature of childhood cancer treatment, the PON must demonstrate a set of clinical competence and technical proficiency that goes beyond general pediatric nursing. This specialization is the bedrock of their practice, positioning them as an indispensable member of the interdisciplinary team.
Advanced Clinical and Technical Proficiency
- The treatments for pediatric cancer—including chemotherapy, radiation, surgery, and especially Bone Marrow Transplants (BMTs)—are complex and carry significant risks.
- Chemotherapy Administration: The PON is the primary administrator of potent cytotoxic agents. This requires advanced knowledge of specific drug protocols, rigorous safety standards (per Oncology Nursing Society guidelines), and the management of central venous access devices (CVADs). Precision in calculation, preparation, and infusion is non-negotiable, as even minor errors can have catastrophic consequences for a child’s tiny body.
- Symptom and Side Effect Management: Childhood cancer treatments bring a host of debilitating side effects, from severe nausea and vomiting to life-threatening neutropenic fever, mucositis, and severe pain. The PON must possess expert knowledge in targeted symptom management protocols, utilizing advanced pain control methods and quickly identifying subtle signs of patient deterioration, which is crucial for improving patient outcomes and quality of life.
- Infection and Blood Product Management: Due to compromised immune systems, children with cancer are highly vulnerable. PONs are experts in meticulous infection control and the rapid, safe administration of blood products (plKnown to meates, red blood cells), demanding specialized training in hematology and transfusion reactions.
The Art of Support:Challenges of Pediatric oncology Nurses, Communication and Emotional NavigationW
While technical skills ensure physical safety, the “art” of pediatric oncology nursing focuses on emotional well-being and reducing the patient’s and family’s barriers to care. This is the Dual Role in action—technical mastery coupled with family-centered care.
-The Role pediatric oncology nurse as “Emotional Anchor“
The PON often spends more cumulative time with the family than any other professional. This proximity makes them the primary source of educational and emotional support.
- Empathetic Communication:
Effective communication is a core competency. This involves active listening, translating complex medical jargon into understandable terms for parents, and communicating truth to children in an age-appropriate, reassuring manner. They must maintain a non-judgmental stance, recognizing that treatment adherence often relies on mitigating family stress.
- The pediatrix Nurse as Navigator:
A crucial, value-added function derived from current research is the nurse’s role as a care navigator. The PON coordinates appointments, manages medication schedules across multiple settings (hospital and home), and proactively addresses social, financial, or psychological barriers that could impede treatment. They bridge the communication gap between subspecialists, ensuring a seamless, holistic treatment experience for the child.
– Palliative and End-of-Life Care by PON:
This is arguably the most sensitive area of practice. When curative treatments are no longer viable, the PON (Pediatric Oncology nursing) transitions seamlessly to a focus on palliative care. They must skillfully manage distressing symptoms while supporting families through anticipatory grief and helping them achieve their goals for their child’s final phase of life.
– The Unseen Toll: Professional Resilience and Self-Care
The high emotional stakes and intense workload of the pediatric oncology unit carry a significant psychological resilience demand. This section is vital for achieving topical authority, as it addresses the sustainability of the profession itself.
The Reality of Burnout
Studies highlight that this environment is fraught with emotional labor, and high rates of nurse burnout and job dissatisfaction are persistent challenges. Witnessing the suffering of children and navigating repeated cycles of hope and relapse can lead to compassion fatigue and moral distress.
Commitment to Professional Development: Given the rapid advances in oncology, the need for continuous learning is paramount. High-performing PONs prioritize self-direction of learning, engaging in regular professional development to integrate new therapeutic guidelines and evidence-based practice into their daily routines.
Cultivating Self-Care: For a PON to remain effective, the commitment to self-care is not a luxury—it is a mandatory professional strategy. Health systems must provide robust psychological support, debriefing protocols, and mentorship programs to help these nurses process the emotional weight of their daily work and maintain job satisfaction over a long career.
Conclusion: The Backbone of Hope
The Pediatric Oncology Nurse is the linchpin of the cancer care ecosystem, embodying an essential blend of advanced clinical competence and profound human connection. They are the constant presence who transforms the daunting journey of childhood cancer into a manageable series of steps, walking alongside the patient and family every step of the way.
It is a role defined by extraordinary demands, yet equally rewarded by the deep satisfaction of providing comfort, minimizing suffering, and fighting tirelessly for every child’s future. The professional dedication and resilience of these nurses underscore why they are, without question, the backbone of hope in pediatric oncology.
What is the Average Salary of pediatric oncology nurse?

Given the high level of specialization, responsibility, and emotional labor involved, the compensation for Pediatric Oncology Nurses (PONs) reflects their critical role. Nationally, the average salary for an oncology registered nurse often falls within the range of $80,000 to $115,000 annually, but this figure varies dramatically based on geography, years of experience, and certification (like the CPHON®).
State salaries are primarily driven by the cost of living and the regional demand for specialized nursing. Below is a snapshot of representative average annual salaries across different U.S. regions:
How to be a Pediatric Oncology Nurse?
The 5 essential step to be a PON are
1- Complete a 4 years Bachelor’s Degree
2- Earn an Accredited Graduate Degree (2-3 Years)
3- Complete Required Fieldwork (Clinical Practice)
4- Pass the National Certification Exam
5- Obtain State Licensure

- Be Respectful
- Stay Relevant
- Stay Positive
- True Feedback
- Encourage Discussion
- Avoid Spamming
- No Fake News
- Don't Copy-Paste
- No Personal Attacks

- Be Respectful
- Stay Relevant
- Stay Positive
- True Feedback
- Encourage Discussion
- Avoid Spamming
- No Fake News
- Don't Copy-Paste
- No Personal Attacks